If you are looking for ketamine therapy in Virginia, Maryland, or DC, feel free to contact NOVA Health Recovery at 571-999-2118 or 703-844-0184 or send us a web form. Please include your phone number so we can connect with you.
If you Can Ketamine help treat seasonal depression? | New Depression Treatments | How Ketamine can help treat SAD? | Four causes of Seasonal Affective Disorder | Northern Virginia Ketamine Center or a loved one are suffering from depression, SAD, anxiety, OCD, PTSD, Bipolar Disorder, or chronic pain, consider ketamine therapy for rapid relief of your condition. NO referral is needed. The treatment is not covered by insurance. The treatment is effective in over 70% of treatment resistant patients. If you are located in the D.C., Northern Virginia, or Maryland area, contact us though the following web form below or through our website directly. We also offer oral and home ketamine therapy:
About 70% of depressed patients feel worse in the wintertime. Seasonal Affective Disorder (SAD) is identified as a type of depression – Major Depressive Disorder with Seasonal Pattern in the Diagnostic Manual of Mental Disorders (DSM-5). Patients with this problem feel symptoms when there is less light in the fall and winter months. There is usually improvement in the spring months as the days grow longer. January and February can be the most difficult months and resolution may be seen in the summer, although some patients are seasonally depressed in the summertime.
- 5% of the population suffers from SAD
- Symptoms may last 40% of the year.
- These symptoms may be due to a shift in the biological clock.
- Women are affected more than men.
- The average age is between 18-30 years when it starts
What symptoms are seen in this condition:
- Feeling sad or having a depressed mood
- Changes in appetite; usually eating more and craving carbohydrates
- Loss of energy or increased fatigue despite increased sleep hours
- Increase in purposeless physical activity (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech.
- Feeling guilty or worthless
- Change in sleep with excess sleep being very common.
- Loss of interest or pleasure in activities once enjoyed and anhedonia.
- Difficulty thinking, concentrating, processing information, or making decisions
- Thoughts of self-harm, death, or suicide
Circadian rhythm disruption either by change of daylight, social jetlag (from late night events and TV), shift work, change in seasons, travel, and exposure to artificial lights is a major cause of seasonal depression. These changes in circadian rhythms are associated with multiple mood disorders as mentioned in the links below:
Circadian rhythm disruption and mental health

In fact, circadian rhythm disruption plays a crucial role in the etiology of depression:
Disruption of Circadian Rhythms: A Crucial Factor in the Etiology of Depression

Chronotypes and affective disorders: A clock for mood?

What are the risk factors for Seasonal Depression?
- Family history. People with SAD may be more likely to have relatives with SAD or another form of depression.
- Living far from the equator. SAD appears to be more common among people who live far north or south of the equator due to variations in light.
- Having major depression or bipolar disorder. Symptoms of depression may worsen seasonally when they suffer from another mood disorder.
What else contributes to SAD?
- Melatonin – This hormone plays a role in sleep patterns and mood. It may be overproduced in SAD due to increased darkness:
The circadian basis of winter depression

The above study demonstrated the phase-shift hypothesis for SAD was a likely correlate of depression.
- Low Vitamin D
Vitamin D is believed to play a role in serotonin activity, Vitamin D deficiency and insufficiency have been associated with clinically significant depressive symptoms:
Associations between vitamin D levels and depressive symptoms in healthy young adult women
- Low Serotonin: People with seasonal affective disorder have difficulty regulating the neurotransmitter serotonin, a neurotransmitter believed to be responsible for balancing mood. In one study, people with SAD had 5% more SERT, a protein that assists with serotonin transport, in the winter months than in summer:
______________________________________________________________________
Diagnostic Criteria for a Major Depressive Episode
A. At least five of the following symptoms have been present during the same two-week period, nearly every day, and represent a change from previous functioning. At least one of the symptoms is either:
- Depressed mood (or alternatively can be irritable mood in children and adolescents).
- Markedly diminished interest or pleasure in all, or almost all, activities
- Significant weight loss when not dieting or weight gain or decrease or increase in appetite.
- Insomnia or hypersomnia
- Psychomotor agitation or retardation.
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive or inappropriate guilt.
- Diminished ability to think or concentrate, or indecisiveness.
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
The symptoms are not better accounted for by a mood disorder due to a general medical condition, a substance-induced mood disorder, or bereavement (normal reaction to the death of a loved one).
The symptoms are not better accounted for by a psychotic disorder like schizoaffective disorder.
Criteria for Seasonal Pattern Specifier
Regular temporal relationship between the onset of major depressive episodes and a particular time of the year (unrelated to obvious season-related psychosocial stressors)
Full remissions (or a change from depression to mania or hypomania) also occur at a characteristic time of year
Two major depressive episodes meeting criteria A and B in last two years and no nonseasonal episodes in the same period
Seasonal major depressive episodes substantially outnumber the nonseasonal episodes over the individual’s lifetime
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: American Psychiatric Association, 1994:327. Copyright 1994.
Treatments for SAD include:
- Cognitive Behavioral Therapy (CBT) which is talk therapy. Problems helped by psychotherapy include difficulties in coping with daily life; the impact of trauma, medical illness or loss, like the death of a loved one; and specific mental disorders, like depression or anxiety.
- Spending more time outside in the sun or by a window exposed to sunlight.
- Structured exercise
- Socialization with friends
- Eating well. In particular, a Mediterranean Diet or anti-inflammatory diet.
- Exposure to light therapy through a 10000 Lux light box for 30 minutes in the morning:
Light therapy is used as a treatment for several conditions, including:
- SAD
- Dementia
- Jet lag
- Types of depression that don’t occur seasonally
- Sleep disorders
- Adjusting to a nighttime work schedule
The light box should be used regularly and at the same time each day. The intensity of the light should be 10,000 Lux at a distance of 16-24 inches from you. This is used first thing in the morning. Tanning beds are not effective for this.
Light regulates the circadian rhythm, and morning light therapy helps night owls with delayed sleep phase disorder fall asleep earlier. In primary insomnia, it improves daytime energy, boosts sleep quality, and helps patients fall asleep faster:
The effects of light therapy on sleep problems: A systematic review and meta-analysis
Light therapy has been used in older adults with Parkinson’s Disease, dementia, and cognitive impairment, and it improved mood and behavioral disturbances, but not the cognitive loss or quality of life:
Application of light therapy in older adults with cognitive impairment: A systematic review
The use of morning light at 10000 Lux and increasing evening darkness (or blue filtering lights or Phillips Hue Bulbs) may be an option to increase efficacy. Remember to not turn on lights at night if you wake up from sleep as it may disrupt your sleep rhythm. Consider specialty wall lights to avoid blue light at those times.
For more information about improving your circadian clock and the timing of morning light for you, go to the CET website: Center for Environmental Therapeutics
What is your chronotype? Here is an online test: AutoMEQ
What is your seasonal pattern: AUTO-PIDS
Also note that ADHD can worsen in the wintertime as well. Light therapy has been shown to improve this:
An Open Trial of Light Therapy in Adult Attention-Deficit
This trial demonstrated a shift towards earlier bedtimes and not so much of a mood benefit.
Bright light therapy also helped reduce combat-related PTSD in a recent randomized trial as well:
Bright Light Treatment of Combat-related PTSD: A Randomized Controlled Trial
The light therapy was delivered across all seasons and decreased core PTSD symptoms.
Medication options:
Bupropion has been shown to be effective in the prevention of SAD by starting treatment prior to the winter season.
Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL:

Three prospective, randomized, placebo-controlled prevention trials were conducted on 1042 SAD patients, enrolled in autumn and treated while still well, across the northern US and Canada. Patients received either bupropion XL 150-300 mg or placebo daily by mouth from enrollment until spring and were then followed off medications for 8 additional weeks.
Major depression recurrence rates during the three studies for bupropion XL and placebo groups were 19% versus 30% (p = 0.026), 13% versus 21% (p = 0.049), and 16% versus 31%; yielding a relative risk reduction across the three studies of 44% for patients taking bupropion XL.
Of note, the use of Bupropion for SAD also helps the resolution of sleepiness and fatigue as depression resolves (relative to SSRI’s):
Treatment of MDD with the NDRI, bupropion, resulted in a greater resolution of sleepiness and fatigue than SSRIs treatment.
Ketamine Therapy for SAD
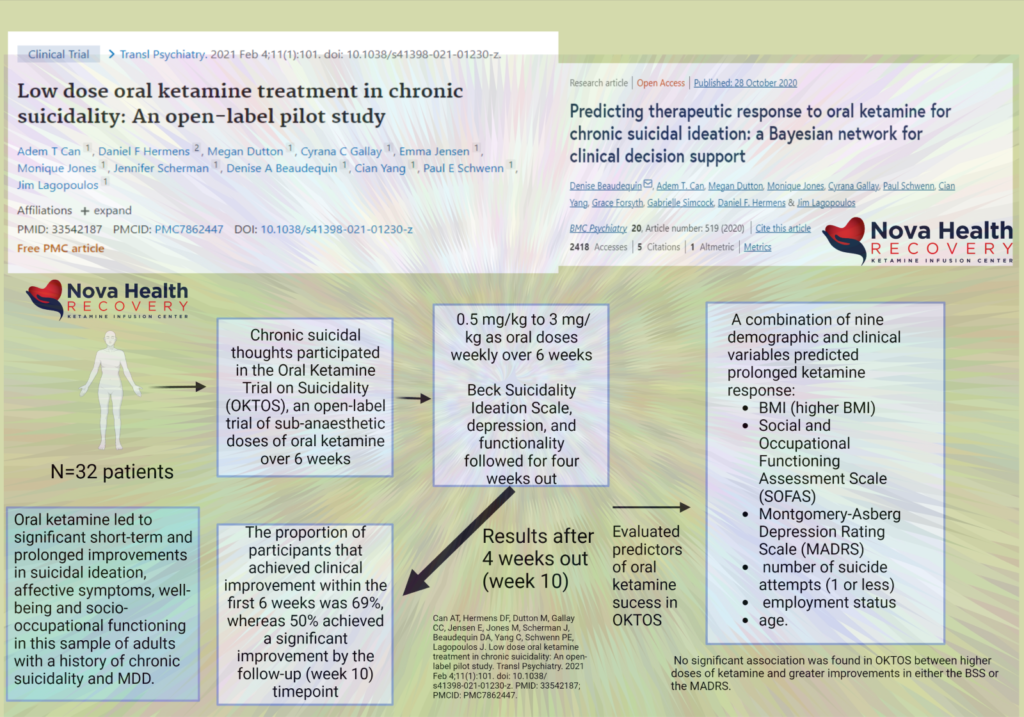
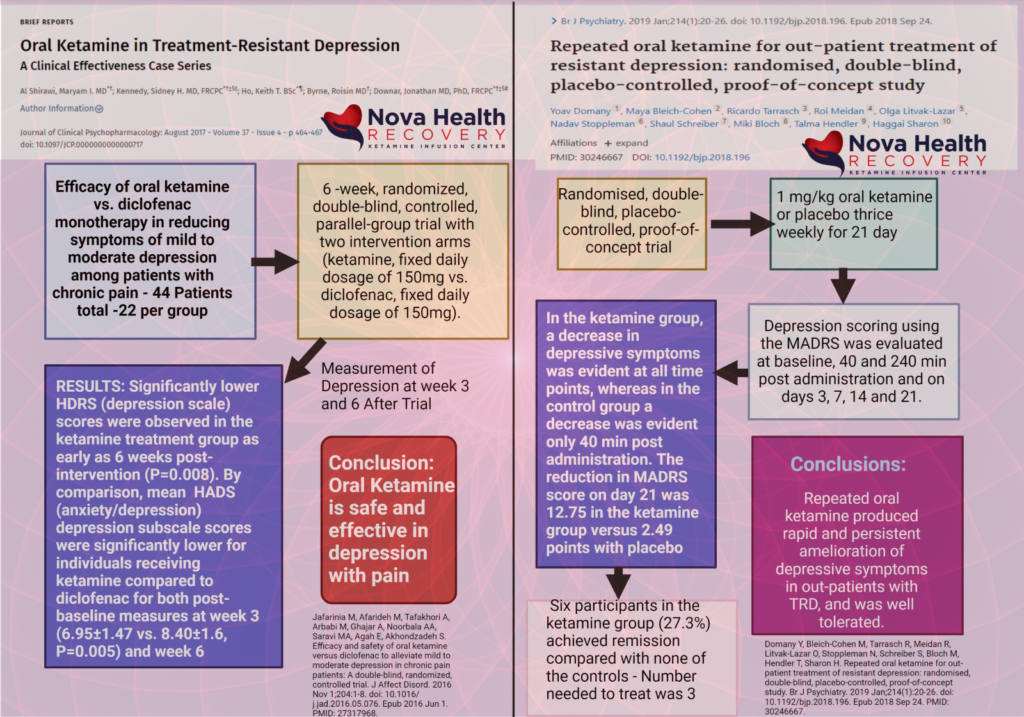
Ketamine also offers a rapid ability to induce mood improvement from seasonal depression. Ketamine, through a series of infusions over two weeks can improve treatment resistant depression in 70% of patients. NOVA Health Recovery Ketamine Center in Fairfax, Virginia offers these infusions with follow-up oral and intranasal ketamine for use at home to maintain effects in combination with other therapies such as light box therapy. Ketamine works well in combination with other modalities and medications.

Ketamine and Sleep: Bridging the Gap in the Treatment of Depressive Illness

Contact Us Here:
National Suicide Prevention Lifeline – 800-273-TALK (8255).